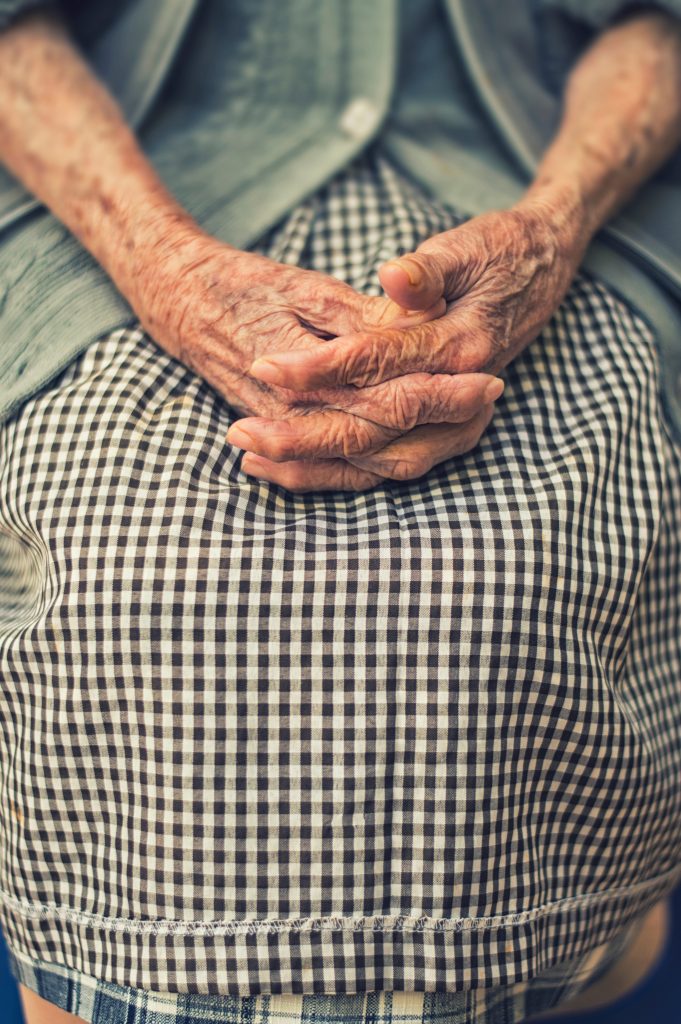
Ageing
Ageing involves many transitions. They can be positive and eagerly anticipated, such as retirement; or they may be challenging and unwanted, such as the diagnosis of a chronic condition with an accompanying deterioration in health and the ability to do hoped for things in retirement.

In Australia the health, disability and aged care sectors are also undergoing transition. They are moving from institutionally directed care models to consumer directed care models. Many older Australians and churches are not ready for those changes and the challenges and opportunities this transition presents.
Faith Community Care can provide innovative responses to older Australians’ community and care needs, and those who are falling through the gaps within other services. Click here to read more including real life examples.
Advance Care Planning
82% of Australians think it is important to talk to their family about how they would want to be cared for at the end of their life. Only 28% have done so. (Dying to Talk)
An Advance Care Plan (ACP) records beliefs, values and preferences, and appoints a substitute decision-maker to take effect when the person is unable to speak up for themselves. This could be due to illnesses affecting cognitive function or the person becoming unconscious. The ACP helps to guide the decisions the health professionals have to make by ensuring the person’s substitute decision-maker is consulted and can convey the person’s values and preferences for their end of life care.

To read more about the ACP and Faith Community Nurses click here
For resources to help with Advance Care Planning and how to start the conversation click here
End of life
The final transition is the end of life. A good death gives the person choices, privacy and dignity.1 It provides a clear understanding of what can be expected, providing access to information and experts who can assist in decision making. People want control over their options – especially regarding pain management, symptom control, the environment in which they will die, and the people who they want to connect with before they die. They want support that addresses their physical, personal, social and spiritual needs.2
Some reflections about how an FCN can journey with someone in the dying process.
Dying Well – what does it mean?
What we understand by a ‘good death’ is influenced by our values, beliefs, culture, faith, life experiences, social supports, and the physical symptoms of our condition. A good death is more likely when we have open and honest conversations about dying with the people we care about. Click here
7 ways to you can help a person die well.
A good death is not just about pain relief and symptom control. Explore seven things you can do that facilitate a person’s good death. Click here
7 things I learned from the ‘Dying Well’ conference Click here
References:
- Smith, R. (2000). A good death : An important aim for health services and for us all. British Medical Journal, 320(7228), 129–130 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1128725/
- Ibid